Introduction
Bone marrow (BM) examination at diffuse large B-cell lymphoma (DLBCL) diagnosis is essential in staging and has prognostic implication. According to the last recommendations (Cheson, et al. JCO 2014) BM biopsy (BMB) is only needed for those patients with a negative BM infiltration by positron emission tomography (PET) for whom identification of occult discordant histology - whose biological and prognostic implications are unknown - is clinically important. Despite its greater sensitivity, flow cytometry (FC) is secondary in BM assessment. Our aim was to compare PET, BMB and FC in the study of BM infiltration at DLBCL diagnosis.
Methods
Retrospective study in two hospitals in Madrid of patients diagnosed with DLBCL NOS from January 2014 to January 2020. A complete BM assessment including PET, BMB and FC was performed in all included patients. The hole series (n=102) was analysed separately according with BM infiltration by each technique, differences between biological, clinical and laboratory variables were studied applying descriptive statistics tests when appropriate (Fisher's exact test, chi-square test, Student's T test and Mann-Witney U test). Event-free survival (EFS) and overall survival (OS) were analysed with Kaplan-Meier estimator according to BM infiltration positive vs negative for each technique, using Cox proportional-hazard model for comparisons.
Results
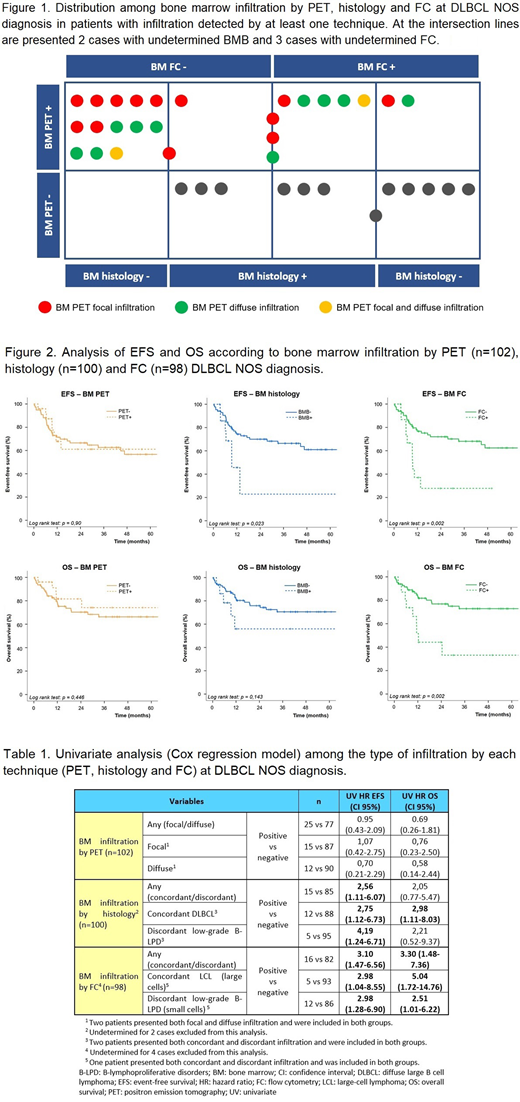
BM infiltration was not assessed in 2 patients by BMB and in 4 patients by FC due to technical reasons. Analysing separately the series according to BM infiltration by each technique (PET+ 25 vs PET- 77, BMB+ 15 vs BMB- 85 and FC+ 16 vs FC- 82) the basal characteristics were comparable between groups, except from extranodal sites ≥2, Ann Arbor III-IV and elevated LDH level in groups with positive BM infiltration. The variables associated with worsen EFS in univariate analysis were age ≥80 years (HR 2.31; CI 95% 1.1-5.1), cell-of-origin (COO) non-GCB (HR 2.33; CI 95% 1.1-4.9), extranodal sites ≥2 (HR 2.39; CI 95% 1.2-4.7), Ann Arbor III-IV (HR 4.55; CI 95% 2.0-10.5), and elevated LDH level (HR 2.32; CI 95% 1.1-4.7). The variables statistically related with worsen OS were COO non-GCB (HR 2.91; CI 95% 1.2-6.8), extranodal sites ≥2 (HR 2.61; CI 95% 1.2-5.5), Ann Arbor III-IV (HR 5.97; CI 95% 2.1-17.3), elevated LDH level (HR 2.36; CI 95% 1.1-5.4), and elevated beta-2 microglobulin level (HR 3.82; CI 95% 1.1-12.9). Double-expressor phenotype did not demonstrated association with EFS or OS. Median infiltration by FC analysis was 0.9% (0.05-27). The series distribution among BM infiltration is presented in Figure 1. Median follow-up was 25 months (0.3-90). Survival curves according to BM infiltration by PET, BMB and FC are presented in Figure 2. Univariate analysis among the type of infiltration by each technique are presented in Table 1. Multivariate analysis included age ≥80 years, COO non-GCB, BM FC+ and IPI score 3-5; BM infiltration by FC demonstrated no association with EFS (HR 2.2; CI 95% 0.9-5.3) or OS (HR 2.5; CI 95% 0.9-6.5).
Conclusions
BM infiltration by PET at DLBCL NOS diagnosis has not survival implication, contrary to infiltration demonstrated by BMB or FC. Cases with positive infiltration by PET but negative by BMB and FC could be false positive in PET or false negative in BMB/FC. According to our results the patients with discordant lymphoproliferative disorder BM infiltration presented worse prognosis and FC is probably the most important technique in this regard.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal